In clinical practice, spinal needle is an important tool used in spinal anesthesia and pain management and for diagnostic lumbar punctures. The spinal needle is a sharp, beveled tip, thin hollow needle used to access and inject anesthetic agents into the cerebrospinal fluid (CSF) directly.
Regional anesthesia require needle and make use of specific part of the body numb to ease pain. It is used in orthopedic surgeries on an extremity, urinary bladder and tract surgery, and female/male reproductive surgery.
Spinal needles are made mostly of high-grade stainless steel for its strength, durability and sterility.
The loss of cerebral spinal fluid cause severe postdural puncture headache (PDPH). Blunt pencil-point tip needles have been found to result to lower risk of of PDPH when compared to similar sized sharp, cutting tip needles. Also, smaller diameter needle cause lower incidence of PDPH.
Spinal needle discovery followed the development of needle and syringes earlier (called hypo-dermic needle in 1859 from Greek origin: ‘hypo’, meaning under and derma, meaning skin).
After the discovery of spinal anesthesia in 1885 by J Leonard Corning, a New York neurologist, different designs of spinal needle have undergone many modifications to improve its application and reduce complications.
There has been alterations to the diameter, tip design and orifice location, to ensure rapid flow of the injected medication and the cerebral spinal fluid (CSF) and also reduce dural trauma and loss of cerebral spinal fluid.
History of Spinal Needle
- In the year 1891, Quincke used a sharp, beveled and hollowed needle to perform the first-ever lumbar puncture.
- Augustus Bier developed a large bore needle (15 to 17G) with a long cutting bevel and sharp point in 1898. However, the large bore causes pain on insertion, and also leaves a large hole in the dura.
- In 1914, Babcock described a needle with a fine cannula that reduced the incidence of PDPH. This needle was a huge success.
- H. E. Greene modified the tip of the spinal needle in 1923. He achieved this by sharpening a 23G cutting needle to a rounded tip by removing the cutting edges of the bevel.
- In 1932, a needle with closed end and lateral orifice was developed.
- Tuohy used a 15G directional spinal needle which he passed a nylon ureteric catheter into the subarachnoid space to enable continuous spinal anesthesia.
- In 1951, Whitacre needle was developed but it has small orifice, with the stylet unable to occlude the orifice. This could cause the orifice to be blocked with tissues.
- Sprotte modified the Whitacre needle in 1987, by increasing the size of the distal orifice to improve the flow of CSF. However, Sprotte needle’s major drawback is incomplete block due to loss of anesthetic drug in the subdural space.
- In 1996, Eldor made the last modification to the spinal needle, by designing a pencil point needle with two lateral holes to allow rapid flow of CSF and distribute the anesthetic agent evenly.
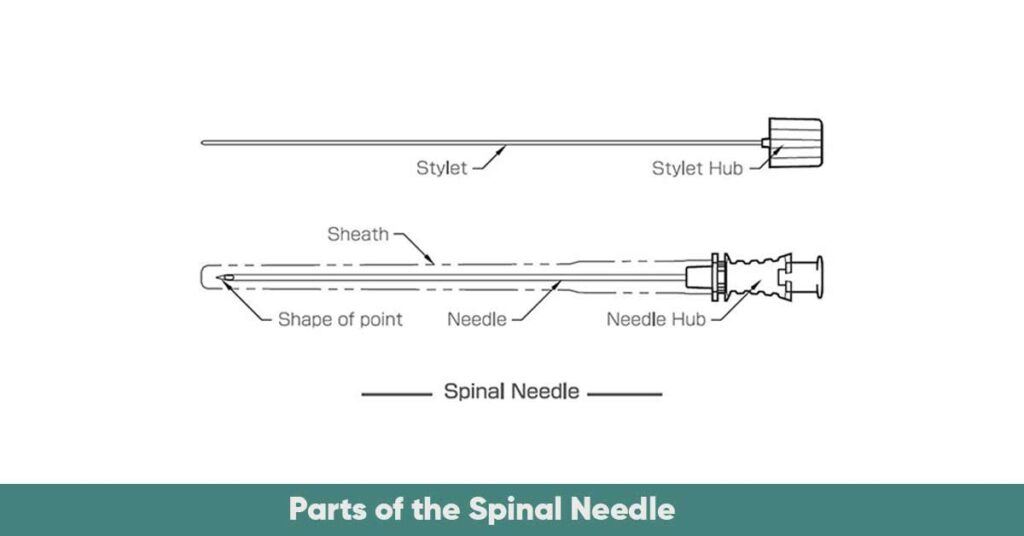
Parts of the Spinal Needle
The major parts of the spinal needle include the tip, the shaft, the hub, and the stylet.
Tip:
The tip can be of two types: the pencil point tip, with blunt, rounded tip that helps it separate tissue gently with less risk of post-dural puncture headache, and the cutting edge tip, with a beveled sharp tip that allows for cutting, used for diagnostics for easy access.
Shaft:
The shaft has varying length and diameter depending on the type of procedure. Thicker needles allows faster flow of medication, while thinner needles cause less tissue trauma.
Hub:
This is the top part of the needle used by the professional for good grip. It is color-coded identifying the gauge.
Stylet:
This is a thin metallic rod within the shaft that prevents the tracking of the epithelial cells into the subarachnoid space and give strength to the needle shaft. Stylets are tight fitting, removable and completely occludes the needle lumen.
Types and Sizes of Spinal Needle
Spinal needle comes in different sizes (16 to 30G), length (5 to 15 cm, with 9 cm length being the most widely used), bevel, and tip design. A 32G design is available but it is less commonly used.
Sizes
The smaller the size of the needle, the lower the incidence of post dural puncture headache. Needles of 24G or lower are mostly used as they cause less headache especially when combined with an atraumatic tip. However, they have less physical flexibility and also slows the rate of fluid flow through them.
Narrow Gauge Needles (25-27 G):
This size is used for diagnostic procedures like lumbar punctures. It is less invasive and causes less lower pain. However, it is difficult to locate due to its small diameter.
Mid – Gauge Needles (22-24 G):
This needle type is used for administering spinal anesthesia, and for pain block. Mid-gauge needles provide a balance between invasiveness and effectiveness.
But it can cause postoperative headache due to the thin gauge.
High Gauge Needles (18-20 G):
High gauge needle is needed when heavy sedation or surgical procedures is indicated, as it can deliver anesthesia or other medications quicker. However, it is more invasive and causes more pain.
Types
Spinal needles are designed in various sizes and gauges. Choice of the needle size depends on factors such as the type of procedure, the anatomy of the patient, and the preference of the physician.
The gauge of the needle is also called as the diameter of the needle, and can affect the flow rate.
Thin needles have higher gauges, are less invasive, and cause less trauma to the tissue, while thick needles have lower gauges but deliver medication faster.
The length of the spinal needle also depend on the patient type, and anatomy, with adults requiring longer needles, while children need shorter ones.
The different types of spinal needles including to the tip design include:
- Pencil Point Needles
- Whitacre
- Sprotte
- Gertie Marx Needles
- Atraumatic Tip Needles
- Cutting-Edge Needles
- Quincke
- Acutip
Pencil Point Needles
These type of spinal needles are conical-elliptical tipped needles (examples include Sprotte and Whitacre), and have advantages such as less trauma, less incidence of PDPH, over the cutting tip needle such as Quincke. They also separate the dura, rather than slice the fibres of the meninges. This allows less leakage of cerebrospinal fluid and promote faster healing.
Whitacre needle:
This type has a rounded, pencil-like point, with small sized non-cutting bevel, and a solid tip. It also has a side injection. This needle minimizes the trauma to tissues, and postdural puncture headache risk compared to Quincke’s needle.
Comes in different sizes such as 27G × 3.5″, 26G × 3.5″, 24G × 3.5″, and 22G × 3.5″. It is used to administer spinal anesthesia in obstetrics.
Sprotte needle:
Identical to Whitacre needle, with blunt round tip, but has a design for smoother and vigorous CSF flow (a larger lateral port). The opening of the hole is wider than the diameter of the needle.
This wide hole allows the local anesthetic agent and the CSF to mix and distribute the anesthetic agent evenly in the subarachnoid space. The elongated tip of the needle helps to ensure gradual separation of the dural fibres causing less CSF leak, and decreased risk of PDPH.
The major advantage is that the size of the lateral hole causes the orifice to straddle the dural layers resulting in the loss of the anesthetic agent, and incomplete block. The width of the hole also leaves the distal portion of the tip prone to risk like damage and fracture.
Used for pediatric and geriatric patients.
Greene spinal needle:
Has a rounded point and rounded non-cutting bevel.
Tuohy needle:
A Tuohy needle is an epidural needle used in spinal anesthesia. It is used when a continuous spinal catheter is to be placed to find the subarachnoid space before placement of the catheter.
Gertie Marx needles:
This type of needle is specifically made for obstetrics, for administering epidural and spinal anesthesia during labor. The pencil-point design and round tip improves labor pain management.
Atraumatic tip needles:
Versatile pencil-point needles designed with blunted tip to reduce trauma in tissues. Used in spinal anesthesia to improve patient’s comfort.
Cutting Edge Needles
Quincke needle:
This is the traditional or standard needle. The very versatile cutting-edge needles have a sharp, easily penetrating needles with a bevelled tip. Caution should be taken to make sure the bevel remain parallel to the dural fibres. Quincke needle comes in sizes such as 29G × 3.5″, 27G × 3.5″, 26G × 3.5″, and 23G × 3.5″.
Used for diagnostic procedure such as lumbar puncture to collect cerebrospinal fluid (CSF).
Pitkin needle:
It has a sharp point and short bevel with cutting edges.
Acutip needle:
The cutting-edge needles are beveled, with sharp tip, designed to enhanced precision and control during specialized diagnostic and therapeutic procedures. However, they may cause trauma in the tissue and PDPH.
Pencil Point Needles
These types of needles are blunted at the point to reduce the incidence of cut that splits tissue but does not traumatic the cells. The design is less likely to cause complications in patients. Examples
Uses of Spinal Needle
- Used for surgical procedures that cut across the lower part of the body like cesarean section
- For chronic pain conditions to administer injections near the spinal column allowing medication closer to the spinal column.
- In diagnostic lumbar punctures carried out to aspirate CSF specimens, particularly to diagnose neurologic conditions
References:
- https://www.gstc.com/types-of-spinal-needles/
- https://www.researchgate.net/profile/Lawrence-Tsen/publication/6918962_Needles_used_for_spinal_anesthesia/links/574618d508ae298602f9efe3/Needles-used-for-spinal-anesthesia.pdf?origin=publication_detail&_tp=eyJjb250ZXh0Ijp7ImZpcnN0UGFnZSI6Il9kaXJlY3QiLCJwYWdlIjoicHVibGljYXRpb25Eb3dubG9hZCIsInByZXZpb3VzUGFnZSI6InB1YmxpY2F0aW9uIn19&__cf_chl_tk=7dgyVLa4JjA7blu1dWK8SIdIATWJcK8hO04vHOEOCEw-1755708090-1.0.1.1-EOfkp69gRG2QIgGOfzOPA8cNFSkz8Uea3tBnqHj_MBg
- https://www.slideshare.net/ZikrullahMallick/spinal-epidural-needle#16
- https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/10.1111/j.1365-2044.2004.03976.x
- https://www.nysora.com/techniques/spinal-anesthesia-2/







