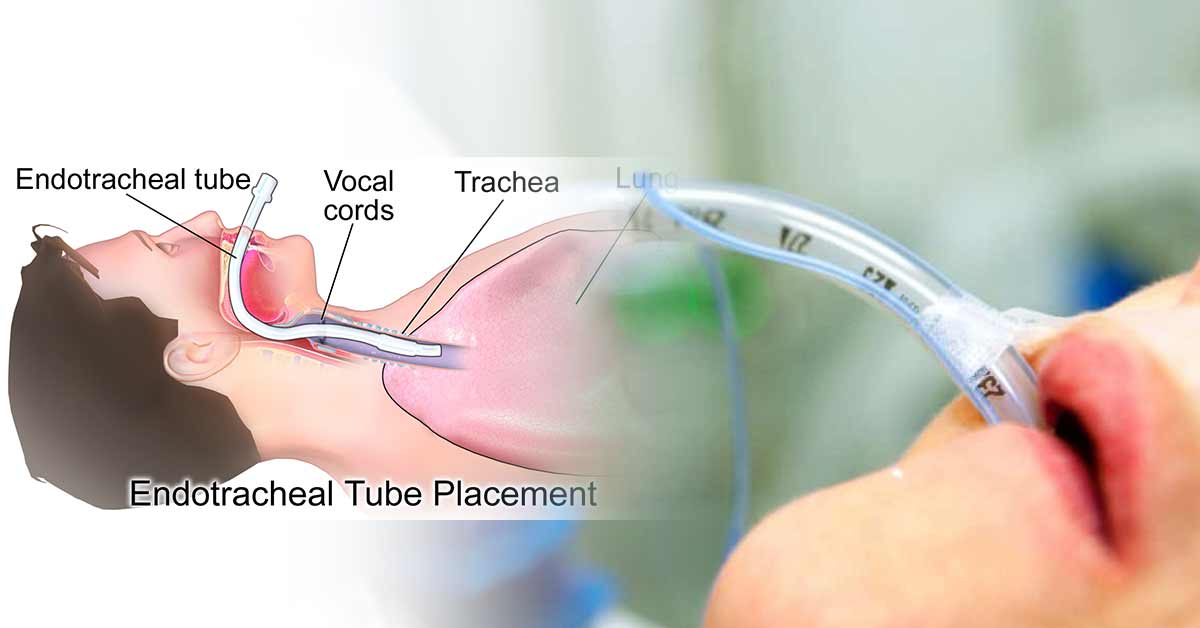
Endotracheal tube is used in clinical setting to provide oxygen and inhaled gases to the lungs, and protect against contaminants like blood, gastric contents. An endotracheal tube is a large-bore
flexible plastic tube placed through the patient’s nose or mouth into the upper part of the trachea above the carina by the way to the voice-box in between the vocal cords to maintain airway.
It is used in general anaesthesia, intensive care and emergency medicine for airway management and mechanical ventilation. Every member of the operating rooms, peri-operative areas, emergency and intensive care units (all places with intubated patients) should know how to place the ETT.
Endotracheal tube was first used in the early 1900s. In the early years, ETT was made from materials like reed, brass, and steel, rubber allowing it to be reused after cleaning and autoclaving.
Now, the ETT is made from mostly polyvinyl chloride (PVC) material, but can also be made from silicone, Teflon, and nylon. This transparent plastic material helps to visualize foreign materials, secretions, and exhalation condensation within the tube.
The PVC tube, in the room temperature, is a semi-rigid material but becomes pliable when it warms after placing in the trachea. It has the advantage of reducing the risk of mucosal ischemia during placement. Also, the tube tip can be easily manipulated during intubation.
Endotracheal tube facilitate the use of inhalation anesthetic, improves oxygenation and ventilation, permits the suctioning of secretions, and reduce the risk of aspiration of gastric contents or oropharyngeal secretions.
Uses of Endotracheal Tube
The main purpose of using an endotracheal tube (ETT) is to secure a definitive airway in both general surgery and non-operating settings for urgent situations.
Securing airway is done due to the inability to maintain airway patency, inability to protect the airway against aspiration, failure to ventilate and oxygenate, and anticipation of a deteriorating course leading to respiratory failure.
Indications:
- Maintenance of airway patency
- For abdominal, thoracic, and neurosurgical procedures
- All head and neck procedures with compromised airway
- For patients with hemodynamic instability, shock, or airway compromises such as stroke, drug overdose, or depressed level of consciousness
- Double lumen tubes are used for intrathoracic surgery.
- Nonsurgical procedure like cardiopulmonary resuscitation
- Decreased consciousness with a Glasgow coma scale (GCS) less than 8, a respiratory rate less than 8c/min or more than 30c/min, PaO2 less than 55 mmHg, PaCO2 more than 55 mmHg, and non-compensated acidosis-alkalosis (Sahiner, 2018).
- Patients requiring Intermittent Positive Pressure Ventilation (IPPV), a type of mechanical ventilation where a machine delivers breaths at a set frequency and volume, which forces air into the lungs to inflate them.
Insertion of the Endotracheal Tube
The distal or tracheal end of the endotracheal tube, also called the patient end, usually comes with an inflatable cuff, and is placed into the trachea. The cuff provides a seal that prevents gastric content aspiration, and also reduces air leakage during positive pressure ventilation. The cuffed tubes are used mostly in patients older than 6 years.
The pilot balloon at the machine end (or proximal end) of the endotracheal tube is used to inflate the cuff. A pilot tube, that runs the length of the ETT, connects the pilot balloon to the cuff. It has a one-way valve which maintains the inflation of the cuff when the inflating syringe is removed.
The endotracheal tube can be beveled or non-beveled. ETT should be removed after the surgery or when there is an improvement in acute illness, mostly within 14 days.
Different Sizes and Types of Endotracheal Tube (ETT)
Sizes of ETT
The size of the endotracheal tube is a measure of the inner diameter of its lumen (millimeters). The different sizes of endotracheal tubes (ETT) ranges from 2.0 to 12.0 mm. Each size has 0.5 mm increase from the previous size.
The choice of the ETT size depends on the height and weight of the patient, the surgery/procedure type, and the presence of airway or pulmonary disease. But since the trachea can vary from patient to patient, several sizes of the ETT should be provided during intubation.
ETT has a depth of 23 cm for men and 21 cm for women, measured at the central incisors. For nasotracheal intubation, 5 cm more is added to this length.
The recommended sizes include:
- Pediatric cases: A formula is used to determine the right size for a child. It is: ID = age in years/4) + 4 for uncuffed ETTs, with cuffed tubes being one-half size smaller. A 10-year-old will likely use a 6.5 size ETT.
- Adult patients: The average size of the tube for an adult male is 8.0, while for adult female is 7.0. The internal diameter for adult male is 8.5–9-mm, while a 7.5- 8-mm internal diameter tube is used for adult females.
- Oral intubation: For women, 7.0-7.5 ETT is recommended, while 7.5-8.5 ETT size ranges are used for men.
- Nasal intubation: A decrease of 0.5-1.0 mm is recommended. The length is proportional to the ETT size. Nasotracheal tubes are shorter than orotracheal tubes by 2 cm in length.
Guide to the Size and Length of ETT in Pediatric Practice
| Age | Weight (Kg) | Size (ID mm) | Size (OD mm) |
| Neonate | 2 – 4 | 2.5 – 3.5 | 10 – 12 |
| 1 – 6 months | 4 – 6 | 4.0 – 4.5 | 12 – 14 |
| 6 – 12 months | 6 – 10 | 4.5 – 5.0 | 14 – 16 |
| 1 – 3 years | 10 – 15 | 5.0 – 5.5 | 16 – 18 |
| 4 – 6 years | 15 – 20 | 5.5 – 6.5 | 18 – 20 |
| 7 – 10 years | 25 – 35 | 6.5 – 7.0 | 20 – 22 |
| 10 – 14 years | 40 – 50 | 7.0 – 7.5 | 22 – 24 |
Types of ETT
- Cuffed vs. Uncuffed: Cuffed ETT has balloon-like cuff at the distal end that inflates creating a seal in the trachea, that prevents air leakage and aspiration. Uncuffed ETT has no cuff and are used mostly in children and for long-term ventilation, where a seal is not needed or when frequent suctioning is necessary.
- Oral vs. Nasal: Oral tube is inserted into the mouth, while nasal ETT is inserted into the nostril.
- RAE tube: The Ring-Adair-Elwyn endotracheal tube. The tube has a bend, typically at a 90-degree angle, to direct the breathing tube and circuit away from the surgical field, especially during oral and maxillofacial surgeries.
- Reinforced tube: The ETT has a wire or coil embedded within the tube wall to prevent kinking or compression, used mostly in head and neck surgeries.
- Laser tube
- Micro Laryngeal tube
- Double lumen tube: Has two separate lumens, which allows ventilation of each lung independently, used especially in thoracic surgery
- Tracheostomy tube: The tube is inserted through a surgically created opening in the trachea (tracheostomy) to maintain long-term ventilation or airway management.
Parts of the ETT
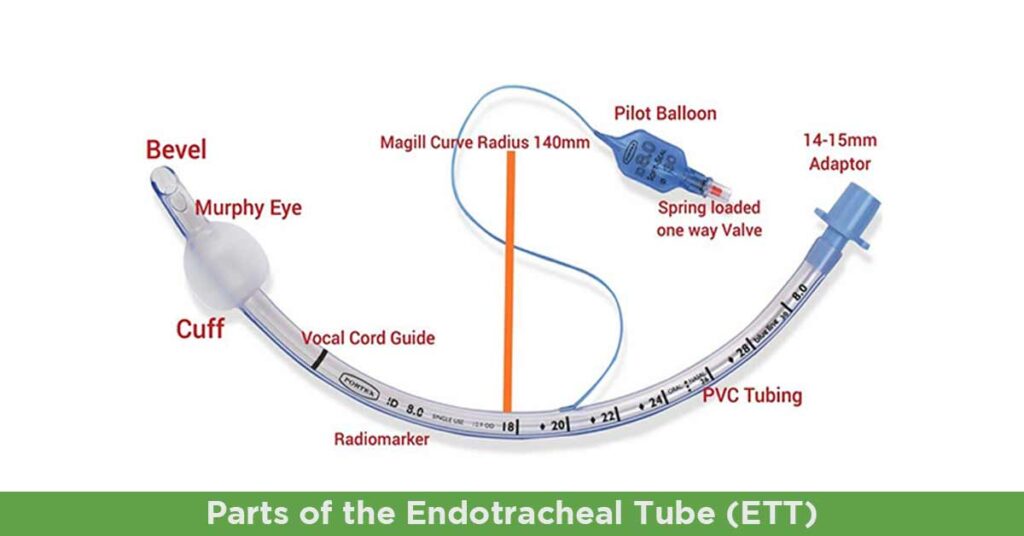
The Tube:
Endotracheal tube has length and diameter. The ETT tube size means the internal diameter in millimeters (mm), with both the inner and outer diameter of the tube listed. For example, a 6.0 endotracheal tube will list both the internal diameter, ID 6.0, and outer diameter, OD 8.8.
Narrower tube has higher resistance to gas flow. So the largest suitable size of the endotracheal tube should be used especially in spontaneously breathing patient who will have to work harder to overcome the increased resistance. For example, a a size 4 ETT has 16 more times resistance to gas flow than a size 8 ETT.
ETT is usually marked in 2 cm increments, and measured from the distal end of the tube.
After the intubation of the patient, the depth of the endotracheal tube ending at the teeth or lips should be noted. This depth will give a baseline measurement ensuring the tube has not moved out of the trachea or deeper into the trachea with the movement of the patient.
A radiopaque linear material is included throughout the length of the tube as the PVC is not opaque, to make it easier to visualize the placement on X-ray.
The Cuff:
This is an is an inflatable balloon at the distal end of the ETT. The cuff produces a seal against the tracheal wall, preventing gastric contents from entering the trachea while enhancing positive pressure ventilation. Pediatric sizes of ETT can come with or without the cuff.
To inflate the cuff, a suitable size of syringe (like 10 to 20ml for adult ETT) is attached to the pilot balloon to provide air under pressure and inflates both the cuff and pilot balloon. After inflating the cuff, the syringe is removed to avoid air in the cuff redistributing back to the syringe and deflating the cuff. Palpating the firmness of the pilot balloon will estimate the pressure in the cuff, with 20 cm H2O or less being the ideal cuff pressure.
The cuff of the ETT is assumed to be non-functional or damaged when the pilot balloon does not hold air. Most ETTs have a low volume, high-pressure cuff, but high volume, low-pressure cuffs are now used recently in modern practice.
High-pressure/low-volume cuffs:
This type of cuff prevent the passing of vomitus, secretions, or blood into the lungs. They exert high pressure on the tracheal wall, but may cause necrosis of the tracheal mucosa, if left in position for a long period of time.
Low-pressure/high-volume cuffs:
They are less capable of preventing the aspiration of vomitus or secretions due to the possibility of wrinkles forming in the cuff. Since the pressure it exert is over a wide area, it cause minimal pressure on the tracheal wall. This allows the cuff to remain inflated for longer periods.
Advantages of cuffed ETT include decreased risk of aspiration, accurate monitoring of end-tidal gases, and tidal volume, and the ability to use high inflation pressures and low fresh gas flows.
The Connector:
The connector attach the ETT to the mechanical ventilator tubing or an Ambu bag. A universal 15 mm connector is used for both adult or pediatric ETTs.
The Murphy’s Eye:
The Murphy’s eye is is another opening in the tube in the distal lateral wall. It is built-in safety mechanism that prevents complete obstruction of the tube. Murphy’s Eye ensures there is still gas flow even if the distal end of the ETT is obstructed by the wall of the trachea or by touching the carina.
The Bevel:
This is a slant that improves the placement through the vocal cords, and helps the visualization ahead of the tip.
Contraindication
Contraindications to placing the ETT include:
- Severe airway trauma or obstruction which prevents placing
- Severe cervical spine injury that requires complete immobilization
- For placement of ETT with nasal approach, contraindications include facial trauma, head trauma as in basilar skull fracture, active epistaxis, expanding neck hematoma, oropharyngeal trauma, and apneic patients.
Complications of Endotracheal Tube
Despite modifications to the endotracheal tube to minimize aspiration, isolate a lung, administer medications, and prevent airway fires, the tube has been implicated in causing ventilator-associated pneumonia.
Other complications include bleeding, infection, perforation of the oropharynx (especially with the use of a rigid stylet), hoarseness (vocal cord injury), and damage to teeth/lips
References:
- https://accessanesthesiology.mhmedical.com/content.aspx?bookid=974§ionid=61588730
- https://www.ncbi.nlm.nih.gov/books/NBK539747/
- https://www.uomus.edu.iq/img/lectures21/MUCLecture_2024_10311448.pdf
- https://www.gimaitaly.com/DocumentiGIMA/Manuali/EN/M34385EN.pdf
- https://mnj.journals.ekb.eg/article_259016_d203235169ba5c3b6fed7b5938b642c2.pdf