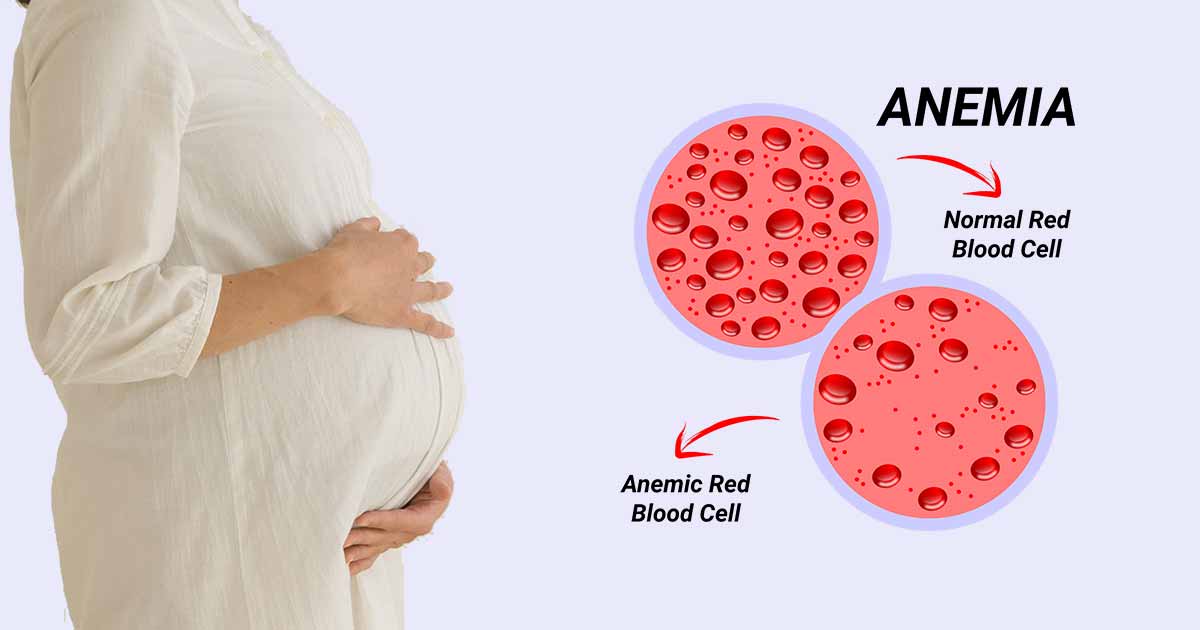
Anemia is a situation in which there is a reduction in the number of healthy red blood cells or the amount of hemoglobin present in the body. Though anemia can affect anyone, but anemia in pregnancy is prominent because this is when the body needs more blood cells and hemoglobin.
During pregnancy, your body stimulates more blood to sustain the growth of the baby. If you are not gaining sufficient iron or specific other nutrients, your body might not be able to produce the number of red blood cells it needs to make this additional blood.
It is usual to have mild anemia when you are pregnant. But you may have more severe anemia from low iron or vitamin levels or other causes.
Anemia can make you feel tired and weak. If it is severe but goes untreated, it can raise your risk of severe complications like preterm delivery.
Types of Anemia in Pregnancy
Several types of anemia can develop during pregnancy. The main types of anemia in pregnancy include:
- Iron-deficiency anemia
- Folate-deficiency anemia
- Vitamin B12 deficiency
Iron-deficiency Anemia
This kind of anemia happens when the body doesn’t have adequate iron to produce good amounts of hemoglobin. Hemoglobin is a protein in red blood cells. It carries oxygen from the lungs to the rest of the body.
In iron-deficiency anemia, the blood cannot carry sufficient oxygen to tissues throughout the body.
Iron deficiency is the most familiar cause of anemia in pregnancy.
Folic Acid Deficiency
It is the lack of folic acid which is the kind of anemia that is second in occurrence. Folates are necessary for appropriate DNA synthesis and amino acid production. Inadequate levels of folic acid may lead to anemia. Folic acid must be supplied in the diet.
Common sources are green vegetables, beans, peas, nuts, fruits (lemons, oranges, bananas, strawberries, melons), and meats (liver, kidney).
Folic acid deficiency is inconsistent and decreased intake is associated with poor nutrition and insufficient absorption, as well as increased folic acid requirement in pregnancy. This is because of the increased demands of fetal growth and maternal erythropoiesis.
Additionally, the increased levels of estrogen and progesterone during pregnancy seem to have an inhibitory effect on folate absorption. The signs of folic acid deficiency are still as exact as general anemia, including roughness of the skin and glossitis.
Vitamin B12 Deficiency
Vitamin B12 is essential for the body to be able to duplicate red blood cells. It is available in animal products, such as eggs, meat, fish, and dairy. It is also available as a dietary supplement and a prescription medication. Fortified breakfast cereals and fortified nutritional yeasts are also good sources of vitamin B12.
Risk Factors for Anemia in Pregnancy
All pregnant women are at risk of becoming anemic. That’s because they need additional iron and folic acid, than normal. But the risk of anemia in pregnancy is higher if you:
- Are pregnant with more than one child
- Have had two pregnancies close together
- Vomit a lot because of morning sickness
- Are a pregnant teenager
- Don’t eat enough foods that are rich in iron
- Had anemia before you became pregnant
Symptoms of Anemia in Pregnancy
The most common symptoms of anemia during pregnancy are:
- Pale skin, lips, and nails
- Feeling tired or weak
- Dizziness
- Shortness of breath
- Rapid heartbeat
- Trouble concentrating
In the early stages of anemia, you may not have noticeable symptoms. And many of the symptoms are ones that you might have while pregnant even if you’re not anemic. So be sure to get regular blood tests to check for anemia at your prenatal appointments.
Risks of Anemia in Pregnancy
The developing fetus depends on you to get enough iron, vitamin B12, and folic acid. Anemia can affect the growth of the fetus, particularly during the first trimester.
If anemia stays untreated, your baby is at higher risk of having anemia after birth, which can lead to developmental issues. Also, anemia raises the risk of delivering your baby early and having a low-weight baby.
Tests for Anemia
During pregnancy, you’ll have a complete blood count (CBC) test done to check if you have anemia at your foremost prenatal meeting. They may also test you toward the end of your pregnancy.
The doctor may look at the quantity and size of your red blood cells, as well as your levels of hemoglobin, ferritin, folate, or vitamin B12.
The medic may then order other tests to determine if you have another type or underlying medical issue.
Preventing Anemia in Pregnancy
Intense anemia during pregnancy is usually treated with blood transfusions. However, anemia is preventable, especially with a diet rich in adequate nutrition.
Below are some ways to make sure you’re getting the essential vitamins and minerals to keep your red blood cell levels within the right span.
Prenatal Vitamins
Prenatal vitamins generally comprise most of the micronutrients that you require during pregnancy, including iron and folic acid.
Taking prenatal vitamins once a day is an easy way to aid boost a healthy diet. It’s ideal to start a prenatal vitamin at least 2 to 3 months before trying to conceive.
Iron Supplements
If you have low iron levels, your doctor may suggest a separate iron supplement in addition to your everyday prenatal vitamin.
You should avoid taking antacids or calcium supplements around the same time as iron supplements, as these may prevent your body from adequately absorbing iron. Taking it with vitamin C will help your body absorb more.
Proper Nutrition
Most people can get sufficient amounts of iron and folic acid during pregnancy by eating the right foods. Good sources of these essentials minerals include:
- Poultry and fish products
- Nuts and seeds
- Dark leafy greens
- Fortified cereals
- Eggs
- Fruits like bananas and melons
Animal sources of iron are the most easily absorbed. If your iron is coming from a plant source, pair it with foods high in vitamin C, like tomato juice or oranges, to enable boost absorption.
Sometimes, supplementing with oral iron is not enough to raise iron levels. In that case, your doctor might talk with you about other therapies. In some cases, intravenous supplementation of iron or a blood transfusion may be necessary.
References:
- GOODLAND, R.D. et al. 1983. Clinical science of normal plasma volume expansion during pregnancy. Am. J. Obstet. Gynecol. 145: 1001.
- https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/